Understanding Revenue Cycle Management
With regards to helping the healthcare industry a few things help take care of Revenue Cycle Management. Let us elaborate a little on the same.
Understanding the Revenue Cycle Management Process is important. So, what is it?
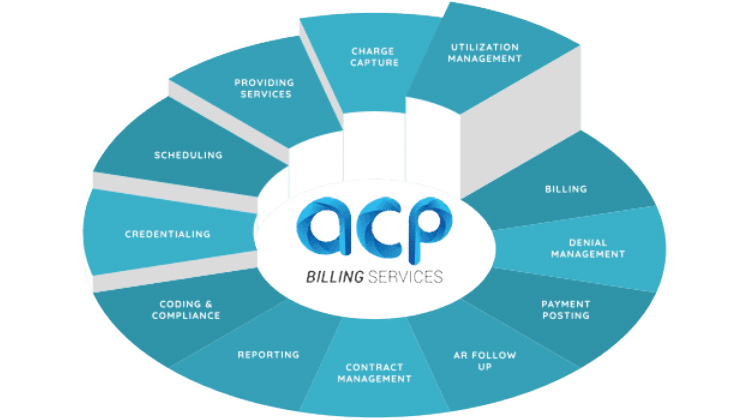
A process in which any practice or health care facility manages functions connected with medical claims processing, payment and revenue including tertiary services such as identification, management and collection of patient services, beginning when an appointment is made by a person and ending when payment is collection.
However, there are still a few steps in between which include the following.
The staffs have to set up the appointments and ensure they have verified the person’s insurance and establish a payment account. In order to optimize the usage of revenue cycle management process pre-registration is vital as, it provides detail medical history and insurance coverage’s about the patient.
Post the appointment registration you get to have a satisfied patient walking out of your office who feels confident of his care your practice creates a claim submission that identifies the treatment received and a code, known as an ICD-10 code, you get to know from this how much the practice should be reimbursed for any specific treatments.
Generating a claim of the patient by the medical practice to a private health insurer or government payer for reimbursement in a manner of speaking sound’s easy however, in reality it is not so as, there are checks or processes that are a pre requisite such as payment posting, processing a statement, collections and claim denial should the need arise.
Post evaluation and once the claim is sent, compensation is given for the services rendered then, there is the possibility of a denial in the claim now this is normally due to the claim being incorrectly coded maybe a chart has information missing or a patient account details is not completed.
The above is just a nutshell and one can be sure to accept that there is a lot more than that.
A strong reason why RCM is a very highly important process and without RCM your practice simply won’t survive. There is also the delay of payments taking months to be resolve with all the back and forth this can be challenging when you are stuck with a patient that needs time to fulfill all the payments needed. In a sense they need to look into their finances credit and insurance history and this is just one of the many challenges associated with RCM.
There is a way where one can save both time and effort in dealing with collections and that’s by collecting payment before the patient leaves your practice. However, some see this as a laborious task as, some patients in an era of rising deductibles cannot afford to pay their bills upfront. The key here is obviously trying to strike a balance in trying to get the patient to make a payment without switching providers as, it could be a future revenue source.
Revenue can be lost if providers can’t identify where issues originated and resolve the same by tracking a claim through its cycle which is a challenge.
The thought of having to train your staff is of course time consuming and a painful one for practices and there is no guarantee that there can be no human errors and this can hamper the schedules for reimbursements eg issues like an incorrect coding.
Here’s how we can help you.
Administrative costs will and overheads will be reduced considerably if we handle your RCM.
We strive to ensure your patients leave with a positive feel of your practice there by raising the bar in terms of customer satisfaction when it comes to billing and insurance resolutions. If your patients are satisfied needless to say they will retain you as a provider.
With the advancement and acceptance of modern technology in RCM, providers today to deal with high readmission rates use telehealth technology this surely cuts down high readmission costs as a major preventing portion which is deemed unnecessary can be avoided and will not hamper the quality of patient care. A branch of the Veterans Health Administration saved more than $150,000 per year in the first two years after it implemented a laboratory expert system, which helps avoid making common mistakes that lead to high-cost behaviors that would aggravate a patient’s patience according to one report.
You can reduce in house Labour costs and increase efficiency can help identify KPIs that determine an organization’s key source of revenue and make continual improvements in services rendered by working with us. It is natural for any health care practice to carefully examine their financial data to make informed decisions.
With the advent of cloud-based RCM and software, our team of billing specialists and managers can help you to effectively handle you practices work and pump up your financial health. Get in touch with us today through any of our social media channels or on our Toll free number – 866-788-5686 and let’s work together so that you can focus on exceptional patient service without billing hassles. ACP – Medical Billing Company in Florida USA
Related Posts
How Revenue Cycle Management Improves Cardiology Billing and Boosts Revenue
Cardiology billing is one of the most complex and heavily regulated areas in medical billing…
How to Effectively Tackle CO 119 Denials: A Comprehensive Guide for Healthcare Providers
CO 119 denials can pose a significant challenge for healthcare providers, especially when a patient…
An Analysis of Key Coding Denial Challenges in Medical Billing
Since revenue cycle management involves a lot of serious steps, many companies prefer to outsource…
Prevent medical billing and coding mistakes
Medical Billing is a very Important aspect in the Healthcare World.






